PRP therapy for joint pain is a groundbreaking, non-invasive treatment using platelet-rich plasma derived from a patient's blood to stimulate tissue repair and reduce arthritis symptoms. Clinical trials have shown its effectiveness in alleviating pain, improving mobility, and promoting new cartilage growth, making it a popular alternative to traditional arthritis treatments.
“Uncover the transformative power of PRP therapy for joint pain as a pioneering approach in cartilage regeneration. This article delves into the mechanics of PRP therapy, exploring its potential in alleviating arthritis symptoms and restoring damaged cartilage. We begin with a fundamental understanding of PRP, its role in regenerating tissues, and its impact on arthritis treatment. Subsequently, we examine the science behind its effectiveness, benefits, safety profiles, and future prospects, offering insights into this promising healthcare innovation.”
Understanding PRP Therapy: A Basic Overview
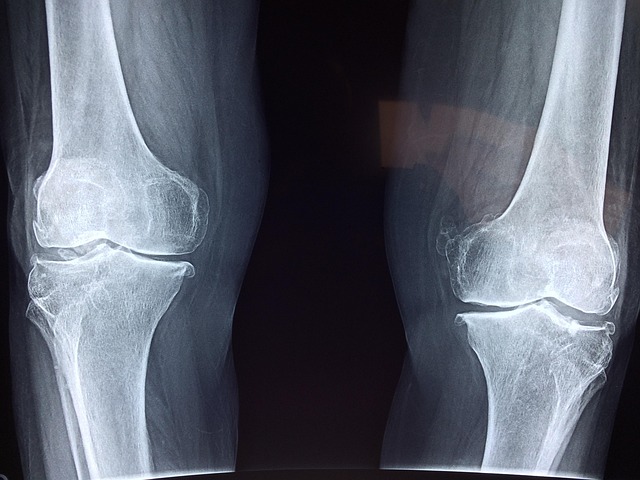
PRP therapy for joint pain has emerged as a promising treatment option, harnessing the power of the patient’s own blood to stimulate cartilage regeneration. This innovative approach involves the extraction of platelet-rich plasma (PRP) from the individual’s blood. PRP contains growth factors and other bioactive proteins that play a crucial role in tissue repair and healing. Once injected into the affected joint, these growth factors initiate a cascade of events, encouraging the body to accelerate its natural recovery process and promote cartilage regeneration.
The procedure is relatively simple: a small sample of blood is taken from the patient, spun in a centrifuge to isolate the PRP, and then carefully injected back into the problematic joint. This minimal invasive technique offers an attractive alternative to traditional arthritis treatments, as it leverages the body’s inherent healing mechanisms without the need for harsh medications or complex surgeries. By stimulating cartilage regeneration, PRP therapy has shown potential in relieving joint pain, improving mobility, and slowing down the progression of arthritis.
The Role of PRP in Cartilage Regeneration
PRP, or Platelet-Rich Plasma, has emerged as a promising treatment option for cartilage regeneration in patients with arthritis. By harnessing the body’s own healing mechanism, PRP therapy for joint pain aims to stimulate tissue repair and promote new cartilage growth. The process involves extracting a patient’s blood and separating it to concentrate platelets, which are rich in growth factors. These growth factors play a crucial role in regulating cell functions and stimulating the production of new collagen fibres, essential for cartilage restoration.
In the context of arthritis, where cartilage deterioration is a significant concern, PRP therapy offers a novel approach. The concentrated platelets act as bioactive signals, attracting stem cells to the damaged joint areas. This cellular recruitment facilitates the formation of new cartilage tissue, helping to restore the joint’s structural integrity and reduce pain associated with arthritis. Studies have shown positive outcomes in clinical trials, making PRP an increasingly popular alternative for managing joint pain and improving mobility.
PRP Therapy for Arthritis: How It Works and Benefits
PRP therapy for arthritis offers a promising approach to cartilage regeneration, targeting the root cause of joint pain and inflammation. This innovative treatment utilizes the patient’s own blood to stimulate healing. During the procedure, a small sample of blood is drawn and spun in a centrifuge to isolate platelet-rich plasma (PRP). Rich in growth factors, PRP is then injected into the affected joint, where it promotes tissue repair and regeneration.
The benefits of PRP therapy for joint pain are numerous. By harnessing the body’s natural healing mechanisms, PRP can help reduce arthritis symptoms, including pain, stiffness, and inflammation. It encourages the growth of new, healthy cartilage, which is particularly beneficial for restoring joint function and mobility. Moreover, as a non-invasive procedure using autologous (self) blood, PRP therapy carries minimal risks and offers a more natural alternative to conventional arthritis treatments.
Safety and Future Prospects of PRP Treatment for Joint Pain
PRP therapy for joint pain has emerged as a promising treatment option, offering a safe and natural approach to cartilage regeneration in arthritis patients. Platelet-rich plasma (PRP) is derived from a patient’s own blood, containing concentrated growth factors that stimulate tissue repair and promote healing. This autologous treatment minimizes the risk of immune reaction or side effects commonly associated with allogeneic treatments, making it an attractive choice for those seeking long-term relief from joint pain.
The safety and effectiveness of PRP therapy have been well-documented in various clinical trials. Numerous studies demonstrate its potential to reduce inflammation, stimulate cartilage repair, and improve joint function in patients with osteoarthritis. As research continues to evolve, the future prospects for PRP treatment look promising. Advanced techniques are being developed to optimize the preparation and delivery of PRP, further enhancing its therapeutic potential. With ongoing studies exploring its application in various joints and conditions, PRP therapy holds great promise as a sustainable and personalized solution for managing joint pain associated with arthritis.
PRP therapy for joint pain shows significant promise in cartilage regeneration, offering a potential game-changer for arthritis sufferers. By harnessing the body’s own regenerative cells, PRP therapy stimulates tissue repair and reduces inflammation. While further research is needed to explore its long-term effects and optimize treatment protocols, the current evidence highlights PRP as a safe and effective option for managing joint pain associated with arthritis. As we navigate this exciting field, ongoing studies will undoubtedly uncover new insights into the potential of PRP therapy for enhancing quality of life for those affected by this debilitating condition.